By: Leslie Shepherd
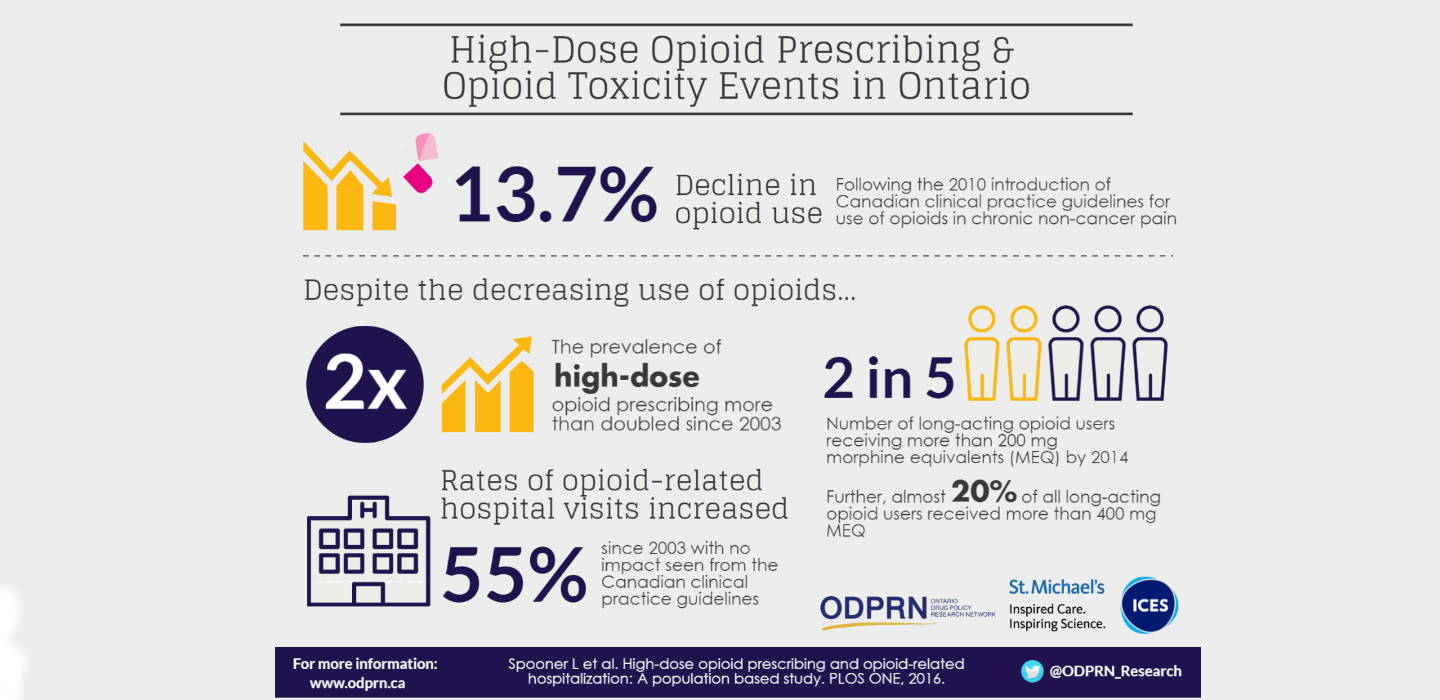
The rate of opioid use in Canada has fallen 13.7 per cent since the publication in May 2010 of national guidelines for their use in chronic non-cancer pain, a new study has found.
Yet rates of opioid-related hospital visits rose 13 per cent between then and the end of 2013 the study found, possibly because people who continue to take some of these potent drugs are often being prescribed high doses, placing them at greater risk of overdosing.
The study, led by Tara Gomes, a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital and the Institute for Clinical Evaluative Sciences, and a principal investigator of the Ontario Drug Policy Research Network, was published today in the open-access journal PLOS ONE.
Gomes and her team examined data for people who were eligible for the Ontario Drug Benefit program between Jan. 1, 2003, and Dec. 31, 2014, and identified 769,895 who were dispensed at least one opioid prescription.
The study found that rates of opioid use remained steady from 2003 until the publication of Canadian guidelines for the use of opioids for chronic non-cancer pain. After this time, the rate fell from approximately 27 per cent of ODB eligible persons in the first half of 2010 to 23 per cent in the second half of 2014.
However, the rate of opioid use was not further affected by the province of Ontario’s enactment of the Narcotics and Safety Awareness Act in November 2011, the study found. A key component of that legislation was the requirement for prescriptions for narcotics and all other controlled substances to be disclosed to the Ministry of Health and Long-Term Care for monitoring and surveillance.
Both the national guidelines and the provincial legislation were designed to promote more judicious and appropriate opioid prescribing, which was expected to reduce the risk of overdoses, as has been seen in some jurisdictions in the United States.
Gomes said that despite decreasing rates of opioid prescribing, among the remaining opioid prescription users, the proportion of high dose use more than doubled from 4.2 per cent in 2003 to 8.7 per cent in 2014.
Canadian national prescribing guidelines currently recommend physicians try to avoid prescribing doses higher than 200 mg morphine or the equivalent in the treatment of chronic non-cancer pain.
In the last six months of 2014, 12,713 people in Ontario eligible for public drug benefits were treated with doses above 200 mg morphine (or the equivalent). Further, the study found 40.9 per cent of recipients of long-acting opioids exceeded daily doses of 200 mg of morphine (or the equivalent) and 18.7 per cent were treated with very high doses exceeding 400 mg morphine (or the equivalent).
Of note, in the last six months of 2014, more than half (55.4 per cent) of long-acting oxycodone users, and more than three-quarters (76.1 per cent) of fentanyl users were treated with daily doses exceeding the Canadian guideline’s upper dose threshold of 200 mg morphine or the equivalent.
The study also found that rates of opioid-related hospital visits increased 34.5 per cent from the first half of 2003 to the second half of 2004, but remained relatively stable between 2005 and 2009. Between 2010 and 2013, rates increased again, rising 13 per cent from 12.4 to 14 hospital visits per 10,000 ODB-eligible persons. The rate of opioid-related hospital visits was not significantly impacted by the Canadian clinical practice guidelines in May 2010 or the Ontario legislation in November 2011. In 2013, there were 1,621 opioid related hospital visits among public drug beneficiaries in Ontario.
“The persistent growth in opioid-related hospital visits in recent years in Ontario could be explained by increased illicit opioid use if people previously using prescription opioids were denied access to these drugs without adequate dose tapering or addiction services,” Gomes said. “Another potential explanation may be dosing errors among people switched from long-acting oxycodone to alternative opioids when formulary restrictions for OxyNeo were introduced in February 2012.”
Gomes noted that one limitation of this study was that the majority of people eligible for the Ontario Public Drug Program are socioeconomically disadvantaged, so the findings may not be generalizable to the overall population. Despite this limitation, she suggested that these findings provide valuable information for physicians and policy-makers as they work toward improving opioid drug policy and appropriate prescribing practices in Ontario.
This study received funding from the Ontario Ministry of Health and Long-Term Care.
This paper is an example of how St. Michael’s Hospital is making Ontario Healthier, Wealthier, Smarter.
About St. Michael’s Hospital
St. Michael’s Hospital provides compassionate care to all who enter its doors. The hospital also provides outstanding medical education to future health care professionals in 27 academic disciplines. Critical care and trauma, heart disease, neurosurgery, diabetes, cancer care, care of the homeless and global health are among the hospital’s recognized areas of expertise. Through the Keenan Research Centre and the Li Ka Shing International Healthcare Education Centre, which make up the Li Ka Shing Knowledge Institute, research and education at St. Michael’s Hospital are recognized and make an impact around the world. Founded in 1892, the hospital is fully affiliated with the University of Toronto.
About ICES
The Institute for Clinical Evaluative Sciences is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Media contacts
For more information or to arrange an interview with Tara Gomes, please contact:
Leslie Shepherd
Manager, Media Strategy, St. Michael’s Hospital
416-864-6094
shepherdl@smh.ca
Deborah Creatura
Media Advisor, ICES
(o) 416-480-4780 or (c) 647-406-5996
deborah.creatura@ices.on.ca
