Critically ill patients admitted to the Intensive Care Unit (ICU) with acute respiratory failure or other critically ill conditions are connected to a mechanical ventilator to support their breathing until they recover from their illness. Mechanical ventilators help the lungs inflate by forcing air into the lungs using positive pressure to facilitate gas exchange. Based on the severity of a patient’s condition, clinicians adjust the ventilator to deliver specific types of breathing patterns according to the volume of the breath, the frequency of the breath, and the amount of effort required by the patient to initiate the breath.
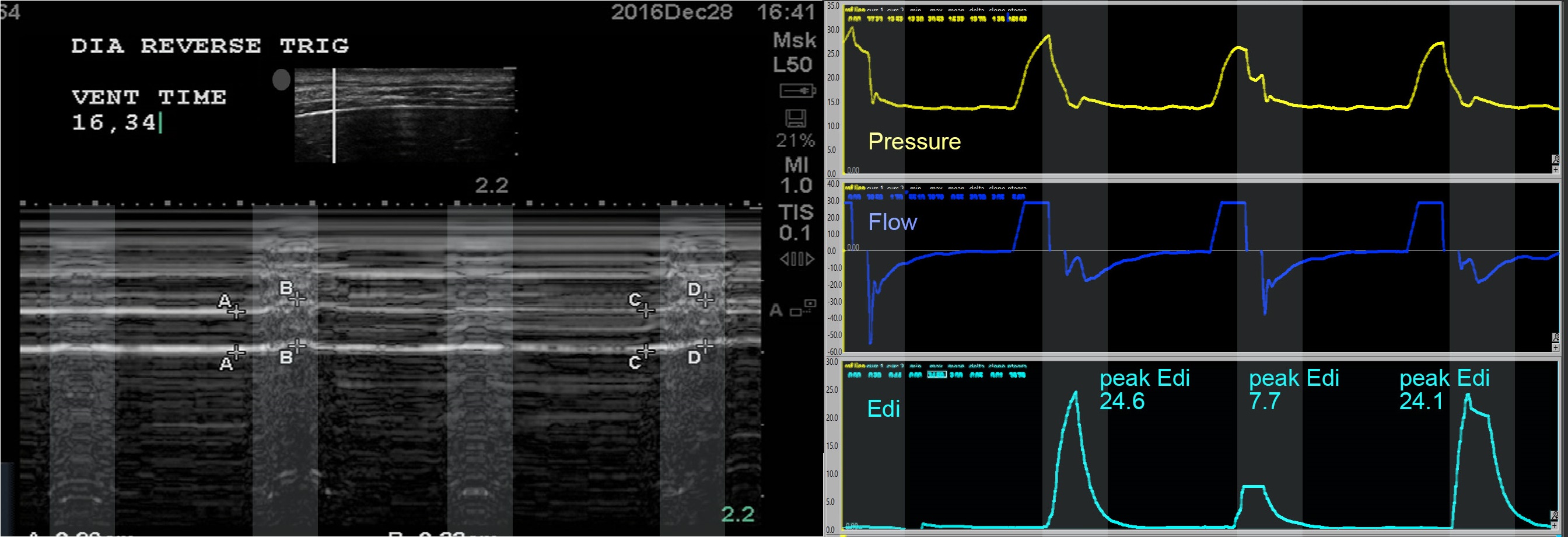
Figure 1: Example of multimodality monitoring of patient-ventilator interactions (ultrasound, airway pressure and flow, electrical activity of the diaphragm) in a patient having reverse triggering.
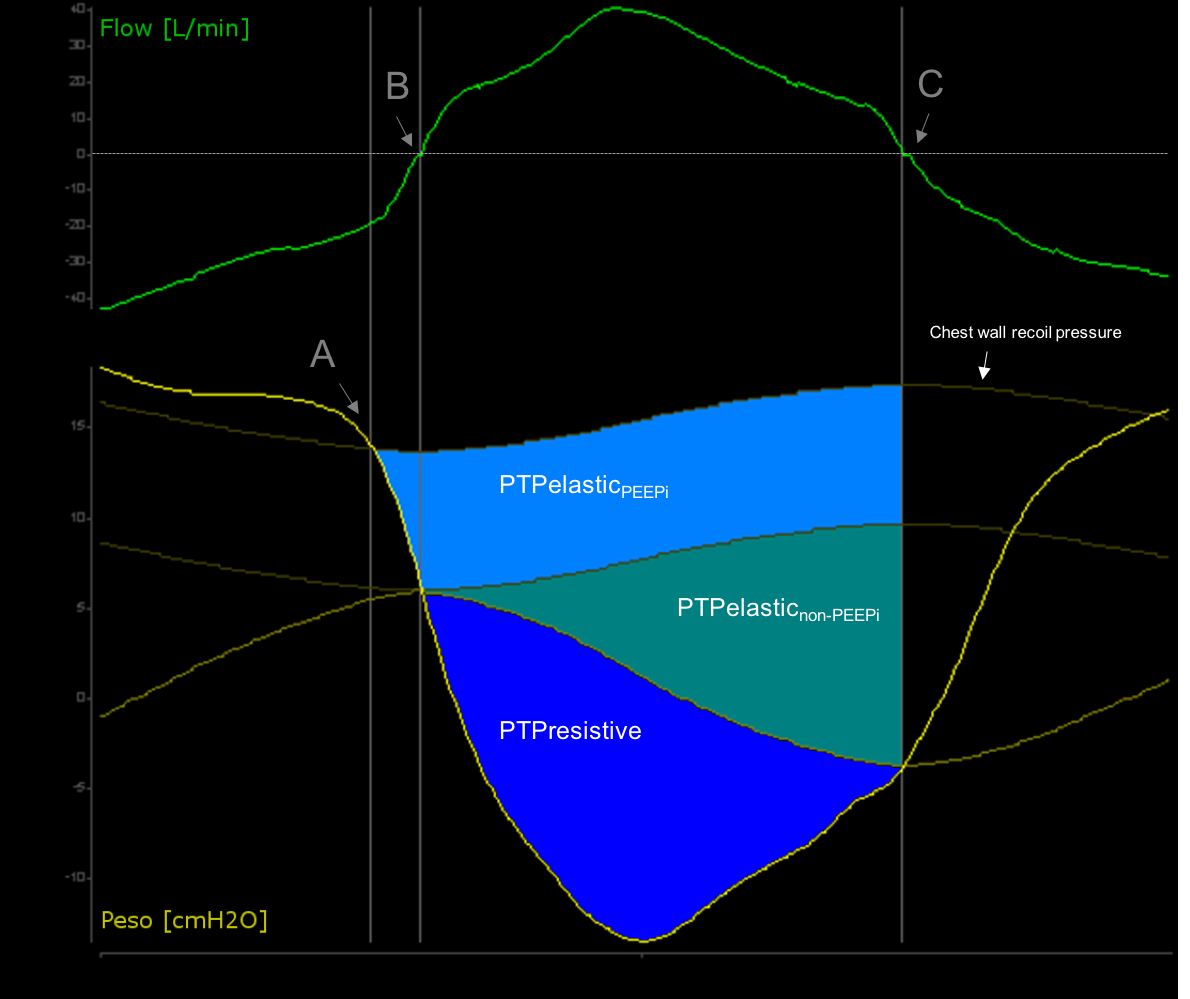
Figure 2: Flow and esophageal pressure (Peso) tracing of a spontaneous breathing patient. The pressure-time product diagram (PTP) is calculated as the area (integral) between Peso and the chest wall recoil pressure.
At an early stage in situations like the acute respiratory distress syndrome, we try to understand how detailed respiratory mechanics assessment can help us to better manage patients and indicate when new techniques are required like extracorporeal circulation.
From observing the interactions between mechanical ventilation and patients’ lungs and breathing we have made enormous progress in our understanding of the pathophysiology of acute respiratory failure over the last 20 years.
We also learned that the interaction between the patient and the ventilator has a huge influence on 1) lung function, 2) respiratory muscles (including diaphragm) function; 3) patients ‘outcomes including duration of ventilation and mortality.
But there is still so much to learn and to improve!
The different modes of mechanical ventilation (i.e., the way in which the ventilator delivers a breath to a patient) and the goals of mechanical ventilation evolve throughout the different phases of critical illness based on the changing demands of the patient and the magnitude of ventilator assistance required. We focus our research on understanding these interactions and finding the best way to optimize mechanical ventilation at all stages. We are interested in the implications for all organs, primarily the lungs but also the respiratory muscles, the circulation, the brain (sleep), etc.
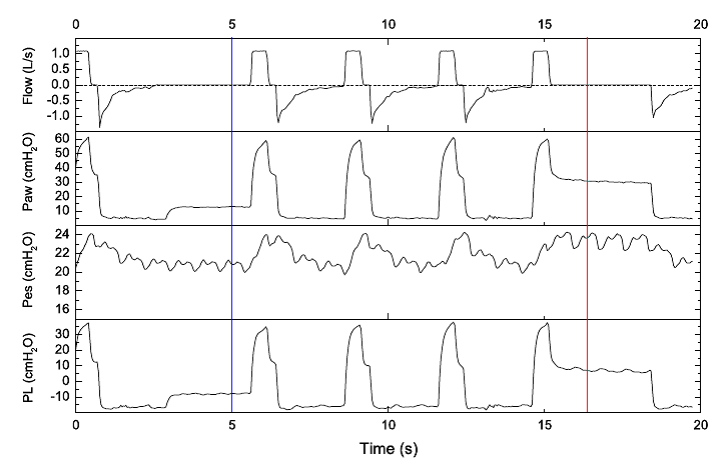
Figure 3: Example of tracings of respiratory mechanics, including esophageal and transpulmonary pressure, in a patient with ARDS.
Video 1: Dr. Tài Pham and Dr. Laurent Brochard present their article -Mechanical Ventilation: State of the Art. This article can be found here.