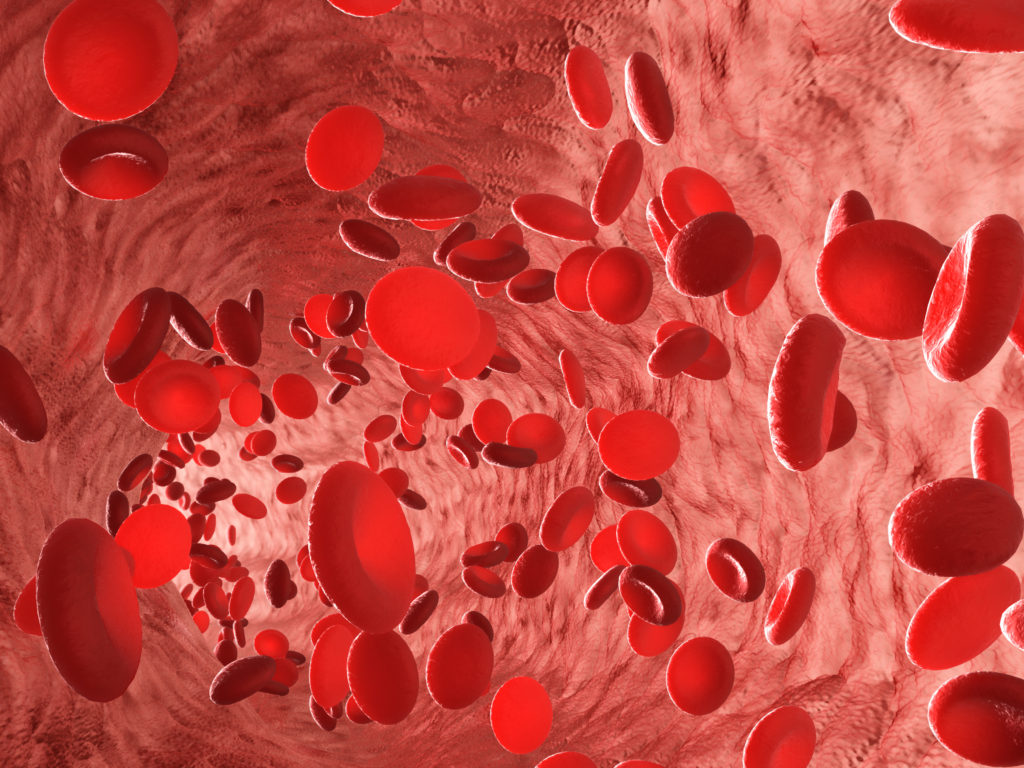
Red blood cells erythrocytes in interior of arterial or capillary blood vessel. Showing endothelial cells and blood flow or stream. Human anatomy model 3D visualization.
A new study published today found that a newly discovered gene helps grow blood vessels when it senses inadequate blood flow to tissues.
The research, published online in the prestigious Proceedings of the National Academy of Sciences, was led by Dr. Philip Marsden, a clinician scientist in the Keenan Research Centre for Biomedical Science of St. Michael’s Hospital, and Dr. Jeffrey Man, a researcher in his lab.
Dr. Marsden and his team set out to better understand how blood vessels regulate the delivery of blood and nutrients to tissues and organs, and how to improve healing after injury caused by inadequate blood flow.
The findings are important because they could help scientists better understand cardiovascular diseases such as heart disease and strokes, which result from inadequate blood flow. The information could also lead to advances in efforts to grow replacement organs or to block blood vessels in tumours.
Dr. Marsden’s lab studies endothelial cells, the cells that line the inside of blood vessels. For this study they looked at a newly described group of genes called long non-coding RNAs, or lncRNAs. RNA, or ribonucleic acid, is found in all cells and it has traditionally been thought that its main job was to carry instructions from genes in DNA to make proteins. But lncRNAs have other roles, including determining the eventual function that individual cells will play in an organism. Studying lncRNAs gives researchers opportunities to find new markers and tests to help make diagnoses for patients.
Dr. Man said this study was the first to identify which lncRNAs are more enriched with endothelial cells compared to other cell types. They plan to make the list public for other researchers to use.
They then discovered that one of those lncRNAs, called STEEL (for spliced-transcript endothelial-enriched lncRNA) was the one that sensed inadequate blood flow in microscopic blood vessels.
“What is really interesting is that STEEL helps our body respond to inadequate blood flow by growing more blood vessels,” Dr. Man said.
“These results show that our bodies are really finely tuned to perform, just as we need them to, and also demonstrate that disruptions to this fine balance can cause problems. This data can be used to improve our understanding of blood vessel diseases and help us find ways to improve healing and recovery after injury.”
This study also made some findings that could be helpful for researchers studying lncRNAs in general, Dr. Marsden said. This study is one of the early studies to assess on a large scale which and how many proteins can associate with an individual lncRNA.
This study received funding from the Canadian Institutes of Health and the Canada First Research Excellence Project.
This paper is an example of how St. Michael’s Hospital is making Ontario Healthier, Wealthier, Smarter.
About St. Michael’s Hospital
St. Michael’s Hospital provides compassionate care to all who enter its doors. The hospital also provides outstanding medical education to future health care professionals in more than 29 academic disciplines. Critical care and trauma, heart disease, neurosurgery, diabetes, cancer care, care of the homeless and global health are among the Hospital’s recognized areas of expertise. Through the Keenan Research Centre and the Li Ka Shing International Healthcare Education Centre, which make up the Li Ka Shing Knowledge Institute, research and education at St. Michael’s Hospital are recognized and make an impact around the world. Founded in 1892, the hospital is fully affiliated with the University of Toronto.
