The idea of ventilating the critically ill has been around since 1543 when Andreas Vesalius proposed “That life may be restored to the animal, an opening must be attempted in the trunk of the trachea, into which a tube of reed or cane should be put; you will then blow into this, so that the lung may rise again and take air.” (1)
Ventilators have helped patients breathe more or less in this way for centuries—filling the lung by force with an amount of air determined by the caregiver.
Even with modern medicine, the risk is that the ventilator is not in sync with the patient’s own breathing efforts. Sometimes, the amount of assist given by the ventilator is set too high, and this can cause lung damage and/or diaphragm disuse, making it hard or impossible to wean the patient from the ventilator. Breathing that is not in line with the body’s needs can lead to discomfort and agitation—requiring painkillers or sedatives—and make it harder to breathe.
Do no harm
The main goals of Critical Care are do no harm and let the patient learn to breathe on their own again.
Drs. Jennifer Beck and Christer Sinderby are a pair of researchers and inventors, both with St. Michael’s Hospital’s Critical Illness and Injury Research Centre. They have reimagined life support ventilators as devices that help the patient get better, with minimal discomfort.
“When people breathe, there are subtle differences from breath to breath because the brain is deciding how much oxygen is needed second-to-second but in Intensive Care Units, the medical team decides how much support the patient needs to breathe, sets the machine to, say, 60 breaths per minute at a fixed pressure,” said Beck. “Christer and our team have developed a way to use signals from the brain to determine how much air is needed each breath and how frequently to deliver air to the patient.”
In healthy people, the brain sends a signal to the diaphragm, telling the muscles to contract and relax—breathing. For critically ill patients, the brain still sends the signal but the body is not able to properly perform the request.
Sinderby had the idea to use the brain’s signal to drive ventilators. Electrodes on the patient’s feeding tube pick up the brain’s signal to the diaphragm and tell the ventilator when and how much to breathe for the patient. Sinderby and Beck have dubbed the approach Neurally Adjusted Ventilatory Assist, or NAVA.
Christer “Columbus”
“He’s Christer Columbus; Jennifer and Christer have discovered an entirely new world,” said Dr. Arthur Slutsky, vice-president of Research at St. Michael’s Hospital and one of the world’s foremost expert in mechanical ventilation. “NAVA has changed the way critically ill patients breathe.”
Since their first publication in Nature of Medicine in 1999, the duo and their team have literally been writing the book, well books, on brain breathing.
They’ve patented 26 inventions thus far. These inventions address the needs of patients of all ages, ranging from premature babies to adults.
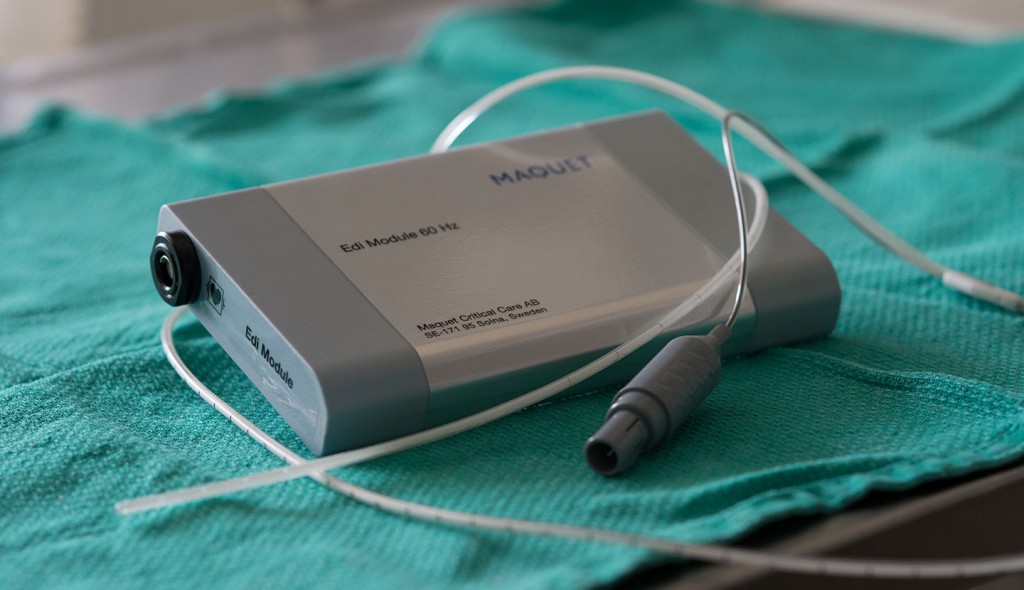
“We of course needed to build some devices that could monitor for brainwaves and deliver breathing support, but the key to our brain-signal-assisted breathing is the NAVA module, the software that translates the signals into information that tells the respirator what to do,” said Sinderby.
The thinker and the tinkerer
NAVA modules resemble a black external hard drive. They are programmed to translate brain signals and instruct the ventilator at the patients beside.
“Whenever Christer gets an idea, we bring it to programmers and mathematicians who make adjustments to the technology,” said Beck. “He moves on to the next idea while the lab and I work to test the updated software and design equipment and processes that will make the NAVA more effective for the critically ill.”
Beck, Sinderby and their team know their roles and have been incredibly successful. The progression of NAVA inventions: idea, patents, testing, patient bedside works for pair—who have been married since 2000.
Another process this team have well-figured out is funding.
A new era of science
The researchers have been validated by uptake of their products. They continue to produce peer-reviewed studies that advance the field of mechanical ventilation that they created. And they have done all this while receiving limited traditional research funding since 2003.
Apart from National Institutes of Health funding in 2003, their lab has been primarily funded by commercialization—the creation of their own research and development company, based in Toronto, and an industry partnership with Maquet in Sweden.
Beck and Sinderby attribute their success to their entrepreneurial spirit.
“You need to be an entrepreneur if you’re going to be successful in science today,” said Sinderby.
Sinderby is presently president of their research and development company, a scientist with St. Michael’s and an advisor to Maquet’s’ Medical Device division. He said it’s unfortunate there is no clear how-to guide for what a researcher does when he or she scores big.
“We’ve been able to keep an active lab where we develop and test many products because we are driven by the market to produce safe technology that meets the needs of patients and healthcare providers,” said Beck.
One thing is for sure, these inventors’ new approach and new technology are helping those with respiratory failure breathe a sigh of relief.
(1) Vesalius A. De humani corporis fabrica. 1543.