Li Ka Shing, Clinical and Population Research Rounds, 2024
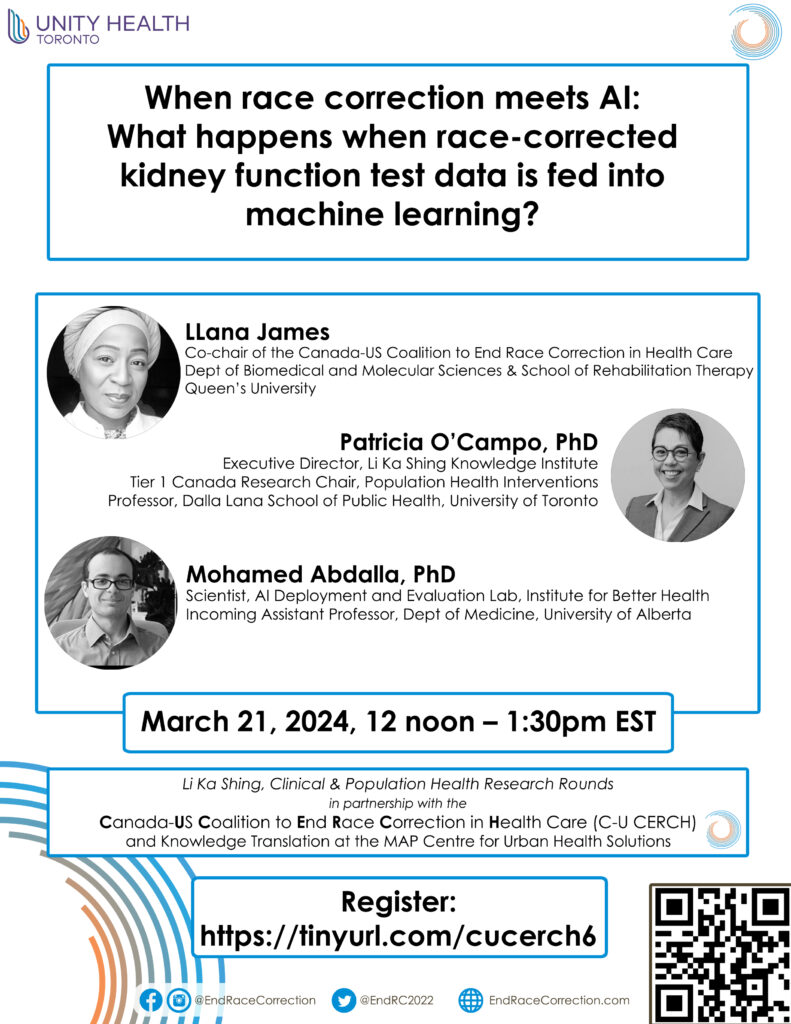
Ending the Practice of “Race Correction” in Health Care speaker series as part of the Li Ka Shing, Clinical and Population Research Rounds, 2024
Presented by Dr. Patricia O’Campo, Executive Director of the Li Ka Shing Knowledge Institute at Unity Health Toronto, in partnership with the Canada-US Coalition to End Race Correction in Health Care and Knowledge Translation at the MAP Centre for Urban Health Solutions.
Date and Time (virtual event): March 21, 2024 from 12 pm – 1:15 pm EST
Registration: https://when-race-correction-meets-ai-uht.eventbrite.ca
About this talk: Computer scientist, Dr. Mohamed Abdalla will consider the implications of feeding data from race-corrected kidney function tests into machine learning applications in hospitals.
Dr. Abdalla will consider this question in conversation with: LLana James (Chair of the Canada-US Coalition to End Race Correction), Dr. Patricia O’Campo, Dr. Gbolahan (GB) Olarewaju and Dr. Nav Persaud.
Background information
What is “race correction”? Health care providers often use tests to assess a patient’s health. In some cases, health care providers calculate test results differently for Black people than they do for everyone else. Overall, “race correction” means that Black people are diagnosed late, or never diagnosed at all, for serious conditions from kidney and lung diseases to cognitive impairment. It also means that Black people are systematically excluded from timely access to life-saving treatments like organ transplants and other surgeries.
What is “race”? “Race correction” has no scientific basis because “race” is not biological. It is a social construct that is applied differently in different times and in different places. In fact, scientists have shown us that people have more in common genetically across “racial” groups than within them.
How does “race correction” work in kidney function tests? The estimated glomerular filtration rate (eGFR) is a test that uses creatinine levels in the blood to estimate how well someone’s kidneys are working. In 1999, clinicians began applying a race “correction” to this test. This “correction” adjusts measurements upwards for people classified as Black by the health care system, which makes them seem healthier than they actually are.
What is the eGFR used for? Medication indication and dosage; referral to a nephrologist by a family physician; referral to specialized chronic kidney disease clinics; referral to dialysis; and, referral for kidney transplant evaluation/access to kidney transplant waitlists.
How does the race correction applied to the eGFR affect Black people? Because Black people’s results are adjusted upwards, “Race-specific inflation can restrict access to treatment at critical junctures by requiring Black patients to reach greater kidney dysfunction before meeting benchmarks of disease” (Tsai et al, 2021). An examination of US health data from 2015 to 2018 found that, without race correction*:
* Uses the MDRD (1999) vs. CKD-EPI (2009) equation based on the fact that the latter was most in use at the time of the study in the US. Both equations apply a race correction.
Tsai, J. W., Cerdeñ, J. P., Goedel, W. C., Asch, W. S., Grubbs, V., Mendu, M. L., & Kaufman, J. S. (2021). Evaluating the Impact and Rationale of Race-Specific Estimations of Kidney Function: Estimations from U.S. NHANES, 2015-2018. EClinicalMedicine.
Is this still happening? In the US, a multi-step, multi-stakeholder task force recommended a new process to estimate kidney function for the US population that does not include a race correction. Implementation of this new process, however, has been extremely uneven. In Canada, there has been a lack of action from health care systems. As a result, in 2020, the Canadian-US Coalition to End Race Correction initiated a multi-step, multi-stakeholder process to update kidney function estimation in Canada. Recommendations and next steps will be provided in 2024.
Speaker bio:
Dr. Mohamed Abdalla is a Scientist at the AIDE Lab in the Institute for Better Health at Trillium Health Partners and incoming Assistant Professor at the University of Alberta. He earned his PhD in Computer Science from the University of Toronto in 2022. His research focuses on the evaluation and deployment of AI in clinical settings.
Moderator and panelist bios
Dr. Patricia O’Campo (moderator) is a Tier 1 Canada Research Chair, Population Health Interventions; a Professor at the Dalla Lana School of Public Health, University of Toronto; and, the Executive Director of the Li Ka Shing Knowledge Institute, Unity Health Toronto. Dr. O’Campo has been widely recognized for her contributions to population well-being through the receipt of early, mid- and late-career awards given by national and international organizations such as the US Centers for Disease Control, American Academy of Pediatrics, American Public Health Association, US Institute of Medicine and the Royal Society of Canada.
LLana James (panelist) is the Chair of the Canada-US Coalition to End Race Correction in Health Care. Her research illuminates how technology can undermine or bolster human rights in the context of clinical care, rehabilitation science and public health. Her interdisciplinary and applied approach is designed to critically appraise current applications of technology while developing and implementing interventions. LLana is also the Health Systems Transformation, AI, Medicine and Rehabilitation Sciences fellow at Queen’s University.
Dr. Gbolahan (GB) Olarewaju (panelist) is a first year Public Health and Preventative Medicine resident. Dr. Olarewaju considers himself an academic activist and his primary research currently focuses on the experiences of Black medical students in Canada and the ways race, racism and health intersect to impact health outcomes. He was the inaugural Chair of the Black Medical Students Association of Canada (BMSAC) and chair of the BMSAC research committee. He continues his advocacy work with various EDI advisory groups for the Faculty of Medicine and as a collaborator on the Canada-US Coalition to End Race Correction in Health Care.
Dr. Nav Persaud (panelist) is Canada Research Chair in Health Justice; staff physician in the Department of Family and Community Medicine at St. Michael’s Hospital, Unity Health Toronto; and, Associate Professor in the Department of Family and Community Medicine at the University of Toronto.
Note: Sign language interpreters (ASL) will be signing during the event.
For any questions please contact LKSKIResearch@unityhealth.to
Below please find important background materials: